Varicose veins are more than just a cosmetic concern. These enlarged, twisted veins are often painful and can lead to various health complications if untreated. While they may appear as bulging, dark purple or blue veins on the surface of the skin, the discomfort they cause can impact a person’s quality of life, affecting activities and even causing chronic pain. For many people, leg pain due to varicose veins is a persistent issue. Understanding the symptoms and treatment options available is crucial for managing this condition and restoring mobility and comfort.
What Are Varicose Veins?
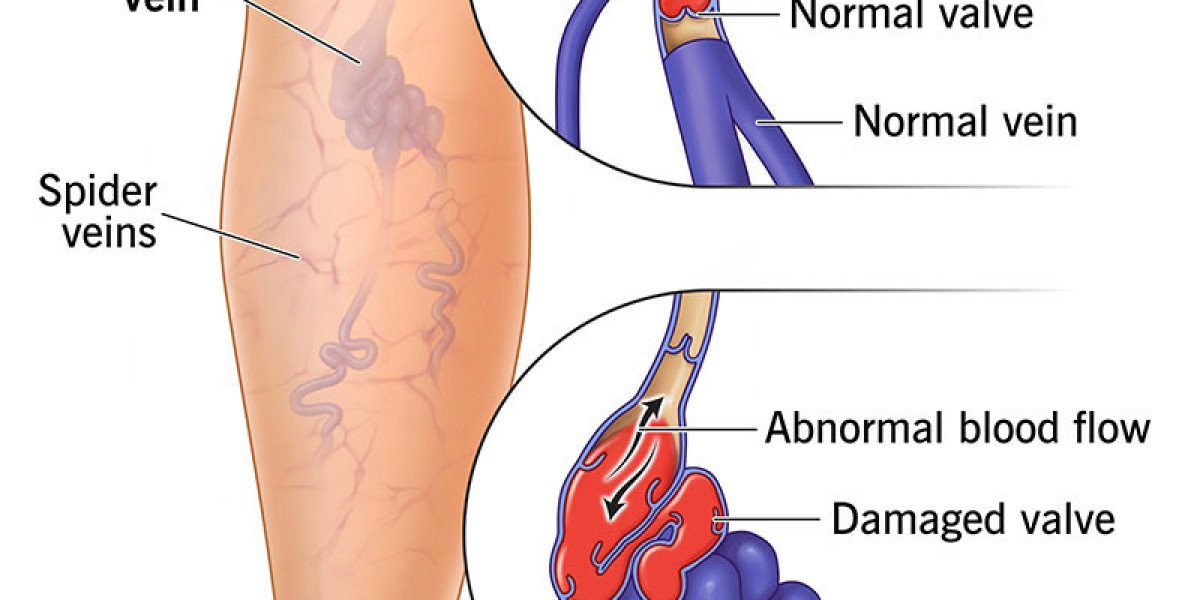
Varicose veins occur when the veins, usually in the legs, become enlarged and overfilled with blood. They often appear swollen, twisted, and raised above the skin surface. The condition is typically the result of weakened or damaged valves within the veins. Under normal circumstances, these valves keep blood flowing toward the heart, but when they malfunction, blood can pool in the veins, causing them to stretch and twist.
Although varicose veins can appear anywhere, they are most commonly found in the legs due to the increased pressure from standing and walking upright. They affect both men and women, though they are more common in women, and certain factors such as age, genetics, and lifestyle can increase the risk of developing varicose veins.
Symptoms of Varicose Veins
While varicose veins are visually noticeable, they often come with a range of symptoms that can impact a person’s comfort and well-being:
Aching Pain and Heaviness: Many people experience a dull, aching pain in the legs, especially after prolonged standing or sitting. This pain often feels like a heaviness or pressure in the affected area and can worsen as the day goes on.
Swelling: Swelling is common around the ankles and lower legs in people with varicose veins, particularly at the end of the day. The swelling results from fluid accumulation due to poor blood flow.
Burning, Throbbing, or Cramping: Some people feel sensations of burning, throbbing, or muscle cramps in the legs, especially at night. These symptoms can disrupt sleep and make daily activities challenging.
Itching: Itching around the veins is also common. This symptom occurs because the stagnant blood irritates the surrounding skin and tissues, leading to dryness and itchiness.
Skin Discoloration: Over time, the skin around varicose veins may change color, appearing brownish or purplish. This discoloration is a result of long-standing venous insufficiency and can be a sign of a more advanced condition.
Ulcers: In severe cases, people with varicose veins can develop ulcers around the ankle region. These open sores are slow to heal and may be painful, potentially increasing the risk of infection.
Causes and Risk Factors of Varicose Veins
Several factors contribute to the development of varicose veins, including:
Age: The risk of varicose veins increases with age, as vein walls and valves weaken over time.
Genetics: If varicose veins run in the family, there is a higher chance of developing them.
Gender: Women are more likely to develop varicose veins due to hormonal changes during pregnancy, menopause, and even menstrual cycles, which can relax vein walls.
Obesity: Excess body weight puts additional pressure on the veins, making it more difficult for blood to flow efficiently.
Lifestyle and Occupation: Jobs that require prolonged standing or sitting, such as teaching, nursing, and office work, can contribute to varicose veins by reducing blood flow.
Understanding these risk factors can help in taking preventive measures to minimize the likelihood of developing varicose veins.
Diagnosis of Varicose Veins
Diagnosis of varicose veins often begins with a physical examination where the doctor examines the affected area while the patient is standing to observe any visible swelling or discoloration. Additional diagnostic tools may include:
Doppler Ultrasound: This non-invasive test uses sound waves to measure blood flow in the veins, helping the doctor determine whether the blood flow is normal or if there’s a blockage.
Duplex Ultrasound: A more detailed form of ultrasound that provides images of blood flow and the structure of veins, helping to identify any issues with the vein valves.
Venogram: In rare cases, a venogram may be performed. This procedure involves injecting dye into the veins to produce X-ray images, showing areas where blood may be pooling due to faulty valves.
Treatment Options for Varicose Veins
Several treatment options are available to relieve leg pain caused by varicose veins, ranging from conservative approaches to minimally invasive procedures. Here are some common methods:
1. Lifestyle Modifications
Compression Stockings: These special stockings help reduce symptoms by squeezing the legs to improve blood flow. They can reduce swelling, aching, and heaviness associated with varicose veins, and are often recommended as a first-line treatment.
Exercise: Regular, low-impact exercise, such as walking, swimming, or cycling, can improve circulation and strengthen the calf muscles, which play a vital role in blood flow.
Elevating the Legs: Elevating the legs periodically throughout the day reduces pressure and promotes blood return to the heart, easing symptoms of swelling and heaviness.
2. Sclerotherapy
Sclerotherapy is a procedure where a solution is injected directly into the varicose veins, causing them to scar and collapse. This process forces blood to reroute through healthier veins, and over time, the treated veins fade away. Sclerotherapy is an outpatient procedure and requires no anaesthesia, with most people resuming normal activities soon afterward.
Advantages:
Minimally invasive with quick recovery time.
Effective for smaller varicose veins and spider veins.
3. Endovenous Laser Treatment (EVLT)
EVLT is a minimally invasive procedure that uses laser energy to seal off the problematic vein. A small laser fiber is inserted into the vein under ultrasound guidance. Once activated, the laser heats the vein’s inner lining, causing it to close. Blood flow then redirects to healthier veins, and the treated vein gradually disappears.
Advantages:
Performed under local anaesthesia.
Minimal pain and short recovery period.
4. Radiofrequency Ablation (RFA)
Radiofrequency ablation is another minimally invasive treatment that uses radiofrequency energy to heat and close off varicose veins. Similar to EVLT, it involves inserting a catheter into the vein and applying heat to close it. Over time, the treated vein shrinks and is absorbed by the body.
Advantages:
Minimal scarring and faster recovery than traditional surgery.
Effective for larger veins, including the great saphenous vein.
5. Venaseal or Glue Therapy
Venaseal, also known as glue therapy, is a modern, minimally invasive treatment for varicose veins. This procedure involves using a medical adhesive to close off the affected vein. A small catheter is inserted into the vein, and the adhesive is delivered to seal it shut. The closed vein is eventually absorbed by the body, rerouting blood flow to healthier veins.
Advantages:
No need for heat, minimising the risk of nerve injury.
No compression stockings required post-procedure in many cases.
Quick recovery, allowing patients to resume normal activities almost immediately.
This technique is especially suitable for patients seeking an alternative to thermal-based treatments.
6. Ambulatory Phlebectomy
Ambulatory phlebectomy is a procedure that removes varicose veins through small incisions in the skin. This is often done for veins that are closer to the skin surface and may be visible as bulging veins. The doctor uses a special hook-like tool to remove the vein segments through the tiny incisions.
Advantages:
Provides immediate relief from bulging varicose veins.
The incisions are small and often leave minimal scarring.
7. Vein Stripping and Ligation
In cases where other treatments are ineffective or when varicose veins are large, vein stripping and ligation may be recommended. This surgical procedure involves tying off the affected veins and removing them through small incisions. Although less commonly performed today, this procedure may still be necessary for severe cases of varicose veins.
Advantages:
Effective for severe cases of varicose veins.
Provides long-term relief, though recovery may take longer than minimally invasive options.
Managing Leg Pain from Varicose Veins at Home
In addition to medical treatments, there are various methods to manage leg pain from varicose veins at home:
Stay Active: Avoid long periods of sitting or standing and incorporate regular, gentle exercises to keep blood flowing.
Wear Compression Stockings: Wearing these stockings daily can help manage symptoms by reducing pressure on the veins and improving blood flow.
Massage: Gentle massage can help reduce swelling and discomfort, but it’s essential to be cautious and avoid applying too much pressure on the veins.
Hydrate and Eat a Balanced Diet: Drinking plenty of water and eating foods rich in fiber can prevent constipation and reduce vein pressure in the lower body.
When to See a Doctor
While some varicose vein symptoms can be managed at home, certain signs indicate that it’s time to consult a doctor:
Persistent leg pain or swelling that does not improve with self-care.
Skin changes such as discoloration or sores near the ankle.
Bleeding from varicose veins, as this may lead to infection.
Development of blood clots, which can cause symptoms like redness, warmth, and swelling in the affected area.
Ignoring severe symptoms can increase the risk of complications, so it’s essential to seek medical attention if any of these occur.
Conclusion
Leg pain from varicose veins can be uncomfortable and may interfere with daily life. Recognizing the symptoms and understanding the treatment options are vital steps to managing the condition. Whether through lifestyle changes, medical interventions like EVLT or RFA, or in more advanced cases, surgery, there are effective options available. Consulting with a healthcare provider can help determine the most appropriate approach based on the severity of the varicose veins, improving quality of life and helping you.